Patient Information Leaflet A1 – Adrenal information
What is an adrenal gland ?
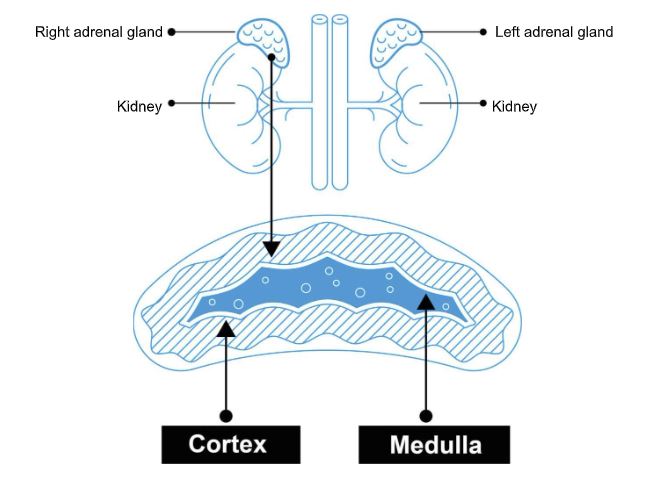
The adrenal gland/s sit above the right and left kidney as shown in the picture. They produce hormones which can affect the body in many different ways
Adrenal secretions
Cortex :
Main secretions : cortisol (affects bone density, glucose secretion, blood pressure) and aldosterone( affects potassium levels and blood pressure)
Other hormones : e.g androgens and female hormones
Medulla:
Hormone secretions; Adrenaline like substances
Adrenalectomy –
Ad/Renal( next to the kidney) Ect/omy ( removal of ) – Removal of the adrenal gland .
Reasons why patients may need adrenal surgery.
The adrenal gland(s) may need to be removed if it has a nodule and / or if it is producing too much hormone. A nodule can also be described as a lesion, lump, mass or tumour. These terms can all be used to describe the same thing and do not give any indication as to the cause of the nodule. Not all adrenal nodules need to be removed as many are benign ( not malignant ) and do not put out extra hormones.
An adrenalectomy may be performed if:
- The nodule/adrenal gland is large in size or growing.
- The cause of the nodule is uncertain on scan.
- The nodule could be malignant (cancerous).
- The nodule is found to make excess hormones e.g.
- A phaeochromocytoma is a tumour that releases too much stress hormone (adrenaline and noradrenaline).
- Cushing syndrome when there are high levels of cortisol caused by the adrenal gland.
- Conns syndrome when there are high levels of aldosterone caused by the adrenal gland.
Investigations that might be performed prior to consideration for surgery
- Bloods for : Cortisol and ACTH(hormone from pituitary gland) , and Overnight dexamethasone suppression test (1 mg dexamethasone at 10pm at night and blood tests at 9 am the next morning)
- Bloods for : Aldosterone and Renin ( aldosterone:renin ratio ), renal profile ( urea, creatinine , potassium, sodium) extra tests may involve a Saline Infusion Test
- Bloods for plasma metanephrines ( adrenaline breakdown products) and /or urinary metanephrines ( 24 hour sample maybe requested)
- Sometimes : DHEAS, androgens, female hormones are tested for as well
Possible Imaging investigations
CTScan : this can either be with or without contrast ( intravenous dye) . This might be to specifically look at the Washout of contrast.
MRI Scan : to look at other characteristics
MIBG Scan: nuclear medicine scan( radioactivity) to look at whether a lesion is secreting adrenaline like products. E.g pheochromocytoma
Other Nuclear Medicine Scans can be used to help look for Conn’s tumours
What type of Adrenal operation ( adrenalectomy) are you likely to expect ?
An adrenalectomy can be performed in a few different ways. Your surgeon will discuss with you which options are best for you and your adrenal gland. Any keyhole operation has a small risk of being converted to an open operation if required to safely remove the adrenal gland. Some hospitals are performing keyhole surgery using robots.
- Laparoscopic (keyhole) adrenalectomy usually involves three or four smaller cuts in the abdomen, approximately between 7- 15mm (less than half an inch) in size. Although one may need to be made bigger to remove the gland through it, depending on the size of the nodule.
- Retroperitoneal (keyhole) adrenalectomy can be performed through the back, through three cuts of approximately 5-10mm. Not all adrenals are suitable for removal this way.
- Retroperitoneal (keyhole ) adrenalectomy can be performed through the lateral aspect of the abdominal wall – through three / four cuts of approximately 5 – 10 mm
- Open adrenalectomy with a larger surgical cut, this may be across the upper abdomen, lateral abdominal wall cut or an ‘L’ shaped cut from the middle of the abdomen to the side the adrenal being removed or a midline incision. This will depend on previous operations, the extent of the operation and also whether other tissues are being removed at the same time.
All keyhole approaches have the possibility of being converted to an open adrenalectomy.
An adrenalectomy is performed under a general anaesthetic and usually takes between one to three hours to do the operation, this is very variable depending on the individual case.
The adrenal gland will be sent for further assessment using a microscope in the laboratory to give more information about what has caused the adrenal lesion. These results will usually be ready about two weeks after the operation and given to you at a follow up appointment.
What will happen prior to your surgery?
Many hospitals have a pre-operative assessment clinic where you will be reviewed by a nurse in preparation for your forthcoming operation.
This or another type of pre-operative check occurs to assess and check whether you are as fit as possible before undergoing surgery. You will usually have some bloods tests, a heart tracing (ECG) and routine health questions, so that if any further investigations or treatment are required they can be arranged.
Someone should be able to advise if you have any queries relating to your medications leading up to your surgery. Usually you are informed as to which medications need to be taken on the day of the operation and which medication should not be taken on the day of surgery ( e.g some diabetic medications, some antihypertensive drugs e.g ramipril )
Some people may need to see an anaesthetist before the day of surgery, others will meet the anaesthetist on the day of surgery.
You may be given a carbohydrate drink to take the evening before the operation and the morning of the operation (unless you have diabetes) to aid with post-operative recovery, and you will be told which of your regular medications you can take before the operation.
Occasionally you may need to be admitted to hospital before your operation, this will discussed with you at the pre-operative appointment and /or with your surgeon.
Is there any extra medication prior to the operation I may require ?
If you are having an adrenal operation for a tumour that secretes extra hormones , you may be asked to take extra medication prior to the operation . Sometimes patients are admitted prior the surgery to stabilise the effects of the hormone secretions. Each hospital adds in extra medication slightly differently. Your surgical /endocrinology team should inform you what is required of you.
How long will I be in hospital ?
This is very variable from hospital to hospital – it can range from a day case to 10 days . Most people will stay around 24 -48 hours. If you have had an open operation, this is likely to be 4- 10 days.
Your blood pressure, temperature and heart rate are likely to be monitored regularly and for some patients this will involve staying in a High Dependency Care Unit initially with closer monitoring.
You may have a catheter (tube in the bladder) placed at the start of the operation, and this will be removed as soon as possible, either at the end of the operation, or if it is needed to monitor how much urine your kidneys are making, it will be removed when you are well enough to walk to the toilet.
If you have a surgical drain (a small tube into the operation site to drain excess fluid away after the operation), it will usually be removed before you go home, and your surgeon will decide when it can come out.
You may experience some constipation, bloating (ileus) or nausea following the operation as the bowel can become sluggish due to handling during the operation or due to pain killers. This often settles with time and constipation can be eased by stool softeners/laxatives, and anti-sickness medication.
We encourage you to get up and about as soon as possible to aid recovery, usually on the first day after the operation, but your surgical team will guide you as to how much to do and when you will be well enough to return to your normal levels of activity.
How soon will I recover ?
This will depend on the extent of the operation . Key hole and robotic surgery tend to be faster than open surgery.
Mobilisation by walking is advised as soon as possible
Following an adrenalectomy, some patients have abdominal discomfort. If you end up taking strong pain killers , constipation can be a side effect and you may require senna and lactulose to help relieve this problem. Tenderness in the upper abdomen and around the scar/s area is common and will disappear in time.
Before resuming driving, you need to ensure that you can wear a seat belt, you feel well enough, you are comfortable enough to perform emergency manoeuvres( (comfortably use the foot pedals ) such as an emergency stop without pain, You should consult the DVLA if you are in any doubt. You are responsible to inform the DVLA.
You should inform your car insurance company that you have had an adrenal operation as different insurers may have their own rules about how long you should wait after an operation before you return to driving. Your return to work depends on the type of work you do and the operation you have had.
You may be able to return to office-based work after one or two weeks and heavier work after four to six weeks. Your surgical team will advise you.
We would not advise anyone to undertake heavy lifting after their operations for at least 6 weeks..
You can ask for a fitness for work note before you leave the ward.
The tumour removed will be assessed by a pathologist for any signs that it may be cancerous (malignant). If it is, you may need further treatment.
Following discharge a Follow up Outpatient Appointment (within 2 months) is likely to be arranged with either your surgeon or your endocrinologists within 2 months after your operation to discuss the findings from the pathology.
Will I need any extra adrenal hormone replacement tablets after my operation?
This depends on which operation you have had performed and what the operation was for.
If you have been found to secrete extra cortisol form your adrenal lesion , you may need extra hydrocortisone after the operation removing this lesion. Some units test the other gland to see how well it is working before you leave hospital ( Synacthen test – this involves an injection and then 2 or more blood tests after the injection ) . Others may give extra steroids and then check later.
If you have been found to secrete extra aldosterone , your renal function and potassium will be watched closely . Very occasionally, some patients are given flurocortisone after the operation.
If you have been found to secrete adrenaline products – sometimes you will need a bit of an extra adrenaline like products support for the first 24 hours – but usually this is not the case.
If both adrenal glands have been removed then you will need to be on lifelong steroid treatment (hydrocortisone and flurocortisone).
- What are the possible complications of adrenal surgery?
The vast majority of patients have straightforward surgery and are discharged without complications. Your surgeon will discuss the benefits and potential complications of surgery with you in detail. Please feel free to ask any questions that are on your mind.
An adrenalectomy is a major operation, and while every care is taken to make it as safe as possible, there are some risks which include:
- Scar(s): This will depend on which operation you are having and the scars have been described above. Some people are more prone to an overgrowth of the scar which can result in a more prominent scar (keloid/hypertrophic scar).
- Bleeding: There is a small risk of bleeding during or after the operation which can sometimes require a blood transfusion or a return to theatre.
- Nerve pain – sometimes nerves in the back and abdomen are irritated by the surgery and you can experience extra tingling and pain around the nerve . usually this will settle down over 6 -8 weeks .
- Infection: Infection is possible with any operation but is not common after adrenal surgery. This can occur in the scar or at the operation site which may need antibiotics or sometimes a drain.
There is a risk of a chest infection, however you can help to reduce this by performing breathing exercises.
If you have a tube into your bladder (catheter) this can also be a possible site of infection. It will usually be removed as soon as possible after the operation.
Damage to nearby organs (uncommon): Any organ near to the surgery has a chance of being damaged. Which organs can be affected, depends on whether your surgery is on the right or the left .
- Right : bowel, kidney, liver, inferior vena cava (large vein going towards the heart), lymphatic channels
- Left : bowel, pancreas, spleen, kidney
However, the chance of damage happening is uncommon.
- Pancreas damage
If the pancreas gets injured this can result in a leak of pancreatic fluid (pancreatic leak) which will need treatment. If there is a suspicion of this , the fluid in a drain or at aspiration will be tested for amylase( an emzyme that the pancreas puts out.)
Sometimes pancreatitis (inflammation of the pancreas) can develop after the operation, this can occur due to moving the pancreas to access the adrenal gland. This is usually mild (unlike other forms of pancreatitis) and does not usually significantly change your post-operative length of stay. - Chyle leak ( lymphatic channels leaking)
This is rarely associated with key hole surgery . however if an extensive operation has been undertaken – sometimes milky fluid comes out through the drain (after you have eaten something ) . if this is the case , the drain is likely to stay in for longer than usual and extra medications and support fluids maybe given - Hernia: This can present as a lump around your scar and if you notice this please inform the team as soon as possible.
- Blood clots: either in the legs (Deep Vein Thrombosis) or lungs (Pulmonary Embolism). This is a risk with any surgery. The risk can be reduced with surgical stockings (worn for six weeks). Injections or tablets of blood thinning medication (e.g heparin) while you are an inpatient and after discharge . You will also be encouraged to get out of bed and mobilise as soon as possible after your operation.
- Need for steroid replacement (temporary or lifelong): Your remaining adrenal gland may be tested after the operation to ensure it is producing enough steroid. There is a small risk you may need steroids after the operation. If however you have Cushing’s syndrome ( excess putting out of cortisol hormones), you are likely to be placed straight onto steroids( e.g hydrocortisone . Steroid production in the other adrenal gland can recover, so the need for tablets scan be temporary. In some cases hydrocortisone can be required for the rest of your life. If you need steroids you will be given further advice and leaflets on this.
Some units undertake a Synacthen test ( injection with a medication that is like ACTH(a pituitary hormone that drives the adrenal to make cortisol) to test whether the adrenal gland that has not been removed is working in certain patients.
- Poor wound healing: This can happen in any wound especially after infection. However, it is more common if you are having the operation for Cushing’s syndrome and if you have diabetes.
- Heart attack/stroke: there is a small risk of heart problems such as a heart attack (myocardial infarction) or stroke with all major operations, but this risk is slightly higher if your adrenalectomy is for a phaeochromocytoma, due to the changes in blood pressure which occur. To help reduce this, you may receive extra medication to control these changes in blood pressure during the operation.
- Risk to your life: adrenalectomy is classed as a major operation, and does carry a small risk to your life.
Most people will not experience any serious complications after surgery.
What will be the result following the operation?
The outcome of your operation will depend on the reason it was performed.
If it is being performed due to Cushing’s syndrome, over the first few months your symptoms such as thin skin, easy bruising, and central weight gain should begin to resolve.
If you have had high blood pressure, blood sugar levels and/or reduced bone density (osteoporosis), these should also improve. Your other adrenal gland will take time to recover its function, sometimes up to 18 months, and during this time you will need steroids.
If it is for Conn’s Syndrome, around two thirds of people with high blood pressure will no longer need medication for blood pressure after the operation. The remaining third would be expected to need less medication for their blood pressure.
If you have a Phaeochromocytoma it is expected that your blood pressure, and sometimes blood sugar levels, and symptoms related to these such as palpitations, headaches, and severe anxiety episodes, should improve after the operation.
These tumours can sometimes recur and you may be kept under follow up for a longer time. You will have an annual blood test to look at your adrenaline/noradrenaline levels.
If it was benign (harmless) you will not require any further treatment.
What is the alternative to adrenalectomy?
If you have a nodule that is producing too much hormone, you may be able to have medication to help control the symptoms and effects.
If you have an indeterminate nodule, there may be an option to monitor the size and growth of the nodule with scans.
You should be able to discuss the risks and benefits of these options with your surgeon.
BAETS information leaflet
Alison Waghorn Dec 2024


